

For patients suffering from thyroid goiters, undergoing surgery can be a daunting treatment. However, for many patients, it’s not the only option. UW Department of Radiology interventional radiologists Sean Golden, MD and Matthew Niemeyer, MD offer thyroid artery embolization (TAE) as a minimally invasive alternative.
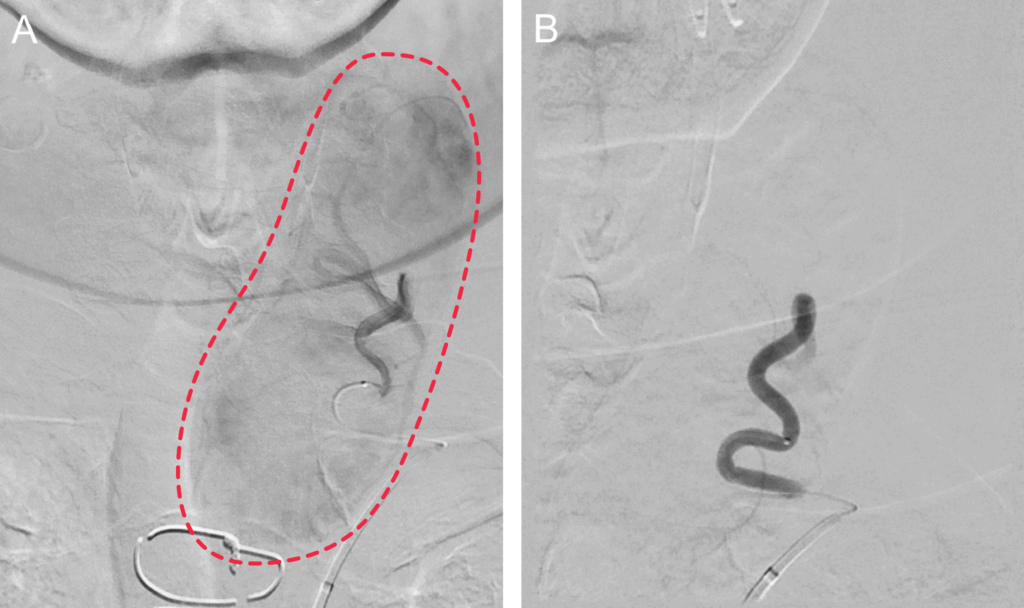
TAE can be a good fit for patients who are hesitant to undergo surgery or have medical conditions that prevent them from doing so. Dr. Golden and Dr. Niemeyer guide a catheter inserted into a small puncture in the patient’s wrist or thigh through the complex network of arteries within the body to those that supply blood flow to the thyroid gland. To help them navigate, the interventional radiologists use fluoroscopy, a specialized live x-ray that shows the catheter moving through the body; similar to how a person can watch their car navigate in real-time on a GPS.
Once they reach the thyroid artery, they inject small particles through the hollow catheter. These particles build up a barricade that blocks the flow of blood, and the restriction of blood flow causes the goiter to reduce in size. Recent cases are showing a 60% reduction in goiter size.
The entire process takes around two hours, and patients can return home the same day they undergo TAE. They may experience mild neck soreness for up to two weeks afterward and should avoid vigorous activities like running for the first week; but are otherwise able to resume their normal daily activities the day following the procedure.
To lay the groundwork for incorporating TAE as a treatment option, Drs. Golden and Niemeyer spoke with interventional radiologists across the nation. Once they’d gained a thorough understanding of the procedure, they connected with endocrine surgery specialist Alex Chiu, MD. A phenomenal collaborator, Dr. Chiu refers patients who are good candidates for TAE. Now that the embolization clinic is up and running, colleagues throughout the institution are referring candidates.
Ensuring the best possible care for patients is a collaborative effort. A multidisciplinary team consisting of surgeons, endocrinologists, and diagnostic neuroradiologists each play a part in the patient’s care journey, from the initial diagnosis and consult through to treatment and post-procedure follow-up.
UW Health is one of the few institutions in the Midwest offering TAE. “One of the great things about UW is that we have access to an amazing hybrid CT angiography room. This allows us to perform a diagnostic CTA prior to embolization so we can confirm blood supply to the thyroid and look for non-target embolization” Dr. Golden explained. “Most other practices use cone beam CT, which provides less detailed imaging. We are researching whether contrast deposition in the thyroid gland on our post-procedure CT predicts the degree of thyroid shrinkage after embolization. We are also researching how long it takes for the thyroid to shrink and alterations in thyroid and parathyroid hormone levels after embolization.”
Physicians interested in learning more can reach the interventional radiology section at 608-263-9729 (ext. 3).