The UW’s Tumor Ablation Lab has been churning out breakthroughs for over a decade, and their current work on tissue response to microwave (MW) ablation could now result in improved ablation antenna design, according to Associate Professor Christopher Brace, Ph.D.
Although radiofrequency (RF) and cryogenic ablation are historical interests of the lab, much of their current work focuses on MW ablation, due to a major federal grant supporting the development and optimization of MW ablation tools. “When we heat cells past 100°C, lots of complex physics are unfolding within that tissue, physics that haven’t been well studied,” said Brace. “Part of our work is to study what’s happening inside the tissue.” Those reactions within tissue have implications for antenna design. Once the tissue surrounding the antenna is heated, the environment around the antenna changes, and the device must be able to cope with those changes.
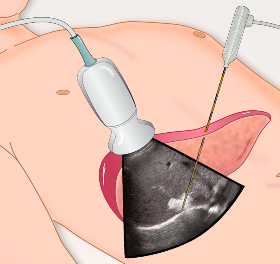
While much of what the Tumor Ablation Lab does is theoretical, the lab is also responsible for a number of devices that have made it to the clinic, and most of them begin the same way by identifying the clinical need. “For example, when we first started working with MW ablation, the existing devices couldn’t make a large enough ablation zone. So our goal was to get as much power into the tissue as possible,” said Brace. They achieved this goal by designing integrated water and gas cooling systems for the antennas, increasing the maximum amount of energy the antenna can impart to the tissue.
After a period of trial-and-error with computer-simulated designs, the lab fabricates prototypes, and begins testing on tissue. Live animal tests are critical in the prototyping stage, as perhaps the biggest factor that impacts the clinical success of ablation devices is the heat carried away by blood perfusion. “We have to do testing in these live animal models to understand how the devices perform in live tissue before we can move into a clinical setting,” said Brace.
Once a prototype passes rigorous testing, the process to take it to manufacture usually involves an outside company such as NeuWave Medical, founded by Brace, Professor Fred Lee Jr., M.D., UW Electrical Engineering Professor Dan van der Weide, Ph.D., and former Tumor Ablation Lab Researcher Paul Laeske. “Technically it’s possible to make something at the university and use it in a patient, but companies can more easily handle the regulatory oversight and process control needed to make a competitive product. They are also the conduit for disseminating the technology to a larger base of physicians,” said Brace. The relationship between the company and the university is collaborative, as UW can be given access to new techniques developed by NeuWave, and if the university develops a prototype device, they can potentially license the design to NeuWave through WARF.
Currently, the Tumor Ablation Lab is also investigating the shrinkage of tissue in response to thermal damage, and how that contraction changes in different types of tissue. This work could result in better guidelines for physicians to use while predicting how tissue will respond to ablation, according to Brace. Other projects involve using ablation not just for tumors, but for treating localized nerve pain and for precoagulating tissue during surgical procedures, a technique known as bloodless resection. These represent new avenues for device design and optimization, providing exciting research directions for the lab.
Read more about the Tumor Ablation Lab.