Contrast Reactions and Pre-Medication – Giuseppe V. Toia, MD, MS
Contrast Reactions and Pre-Medication
Contrast Reactions and Pre-Medication
Lecure on managing contrast reactions.
description of contrast media control systems to assure compliance with JCAHO standards
File: uwhc-contrast-media-control-systems.pdfInstructions and link to exam on uwhealth.org
File: contrast-reaction-test-instructions.pdfExtensive tutorial on contrast agents
File: contrast-agents-tutorial.pdfDrug selection chart for adult patients
File: contrast-rx-dosage-adult.pdfmedication and dosage charts for pediatric patients
File: contrast-rx-dosage-peds.pdfRevised 6/9/2025
Contrast extravasation, also known as contrast infiltration, refers to the unintentional leakage of intravenously injected contrast media from a vein into the surrounding soft tissues. It is a rare phenomenon happening in 0.1 – 1.2% (1/1000 – 1/83) of all CT contrast injections. Extravasations with gadolinium-based contrast media are much less common than those seen after injection with iodinated contrast media but can happen.
Most contrast extravasations resolve without complications. Severe extravasation events are extremely rare happening in <<1% of all extravasations. Severe extravasations can induce compartment syndrome, a painful condition caused by a build-up of pressure in a closed muscle or tissue compartment, potentially restricting blood flow and leading to tissue necrosis, and nerve damage. Other severe reaction sequelae include skin blistering and necrosis. While it was initially hypothesized that larger volumes of extravasated contrast were more likely to cause compartment syndrome, there have been studies showing that small volumes can also cause it, particularly when it happens in less capacious volumes of tissues, such as the wrist or foot. Low- and iso-osmolar contrast agents (e.g., iohexol and iodixanol, respectively) have an even lower chance of causing a severe extravasation event as compared to older high-osmolar agents (e.g., diatrizoate) which are no longer used intravenously.
Extravasations are more common in patients who cannot communicate effectively (e.g., infants, patients with altered consciousness), are severely ill or debilitated, have altered circulation in the injected extremity (e.g., lymphedema, phlebitis, acute trauma), had radiation to an injected extremity, or are injected in the hand, foot, or ankle.
Power injected contrast via flow-rate approved central lines and PICCs also vastly decreases the incidence of extravasations.
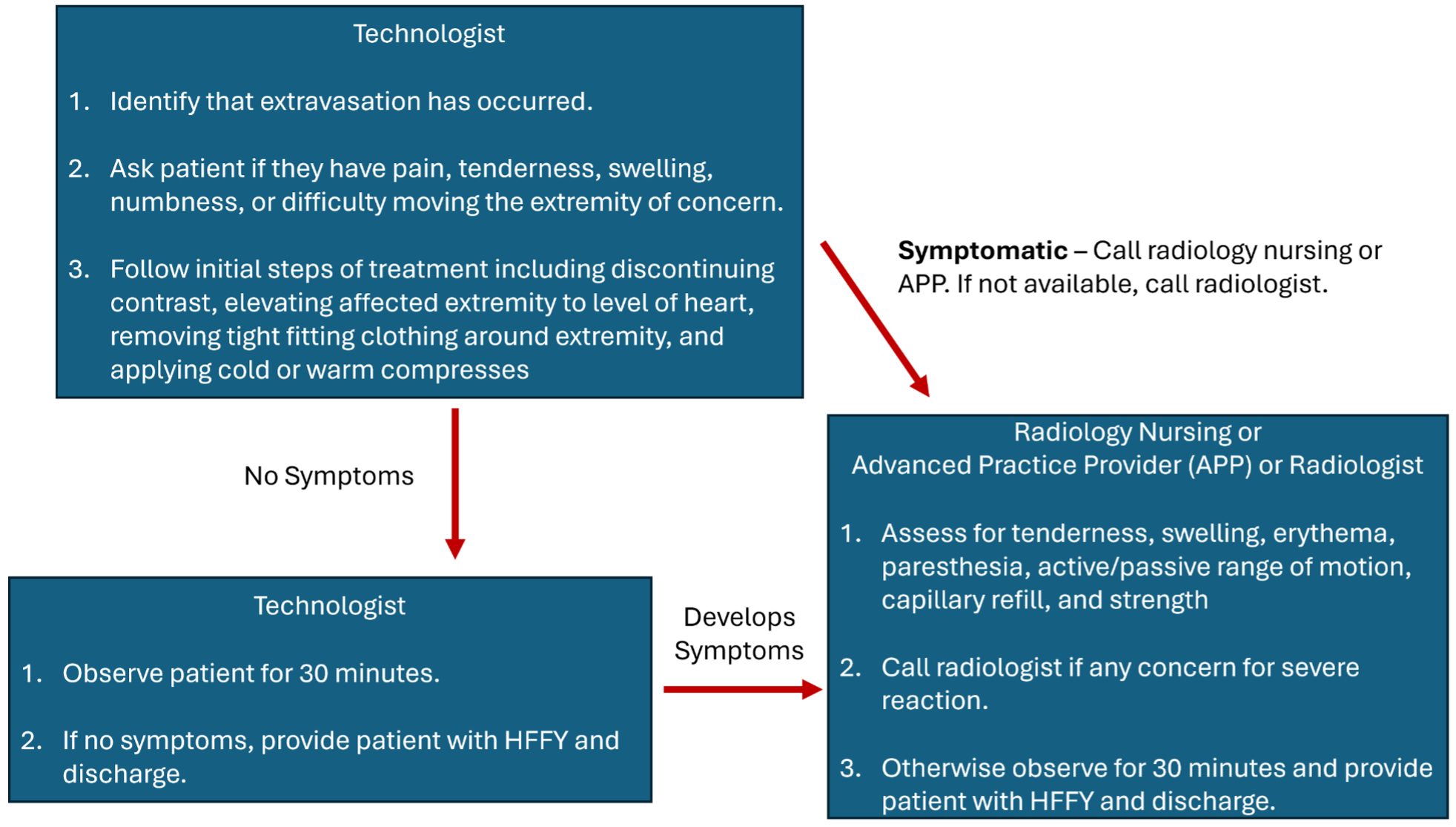
In most patients, initial swelling and tenderness resolve within hours to days after extravasation. Most patients recover without any clinically significant sequelae. If a contrast extravasation happens, use these guidelines (regardless of contrast agent):
An imaging technologist is the first health care provider likely to recognize a contrast extravasation.
If patient does not indicate any pain or discomfort on initial assessment: Technologists observe patient for at least 30 minutes. If patient does not have worsening symptoms, patient can be discharged using the discharge protocol below.
If patient appears acutely symptomatic on initial survey or patient develops worsening symptoms after 5 minutes of observation/treatment or the technologist feels unsure of their assessment (e.g., patient mental status altered and unable to convey symptoms): Technologist should call a radiology nurse or advanced practice practitioner to assess the patient. The technologist should readily convey any clinical information they have gathered once additional health-care providers arrive. If a nurse or APP is also concerned for compartment syndrome, the radiologist should be notified to assess the patient.
If a nurse or APP is unavailable, a radiologist (attending or trainee) should assess the patient.
We stress that compartment syndrome almost always takes time to develop, on the order of hours to days.
.
Purpose: reduce the number of patients with known allergies scanned at East Clinic, Digestive Health Center, and other non-hospital outpatient centers.
7/2020
What patients require premedication prior to IV contrast?
A prior allergic-like or unknown type reaction to the same class of contrast medium is considered the greatest risk factor for predicting future adverse events. Premedication prior to administration of intravenous contrast is recommended in this group of patients.
In general, patients with unrelated allergies are at a 2- to 3-fold increased risk of an allergic-like contrast reaction, but due to the modest increased risk, restricting contrast medium use or premedicating solely on the basis of unrelated allergies is not recommended. Patients with shellfish or povidone-iodine (e.g., Betadine®) allergies are at no greater risk from iodinated contrast medium than are patients with other allergies (i.e., neither is a significant risk factor).
In patients with reported prior contrast allergy or reaction:
Greenberger PA et al. Emergency administration of radiocontrast media in high-risk patients. J Allergy CLin Immunol. 1986; 77(4): 630-634.
Mervak BM, Cohan RH, Ellis JH, Khalatbari S, Davenport MS. Premedication administered 5 hours before CT compared with a Traditional 13-hour Oral regimen. Radiology 2017; 285(2), 425-433..
McDonald JS, Larson NB, Kolbe AB et al. Prevention of Allergic-like Reactions at Repeat CT: Steroid Pretreatment versus Contrast Material Substitution. Radiology 2021; 000:1-8.