History: 41 year-old status post bilateral mastectomies and TRAM reconstructions four years ago for DCIS found on a left breast core biopsy, now with new palpable left breast lump.
Solution: Papillary carcinoma constitutes approximately 2% of all breast cancers. Compared to other forms of breast carcinoma, papillary carcinomas are diagnosed in older women with a mean age of 63-67 years. Clinically, these cancers manifest clinically as a palpable mass or nipple discharge. Often the nipple discharge is blood-tinged. In general, papillary carcinomas are slow-growing. Intracystic papillary carcinomas are associated with a good prognosis (10 year disease-free survival rate of 91%). Axillary metastases are infrequent.
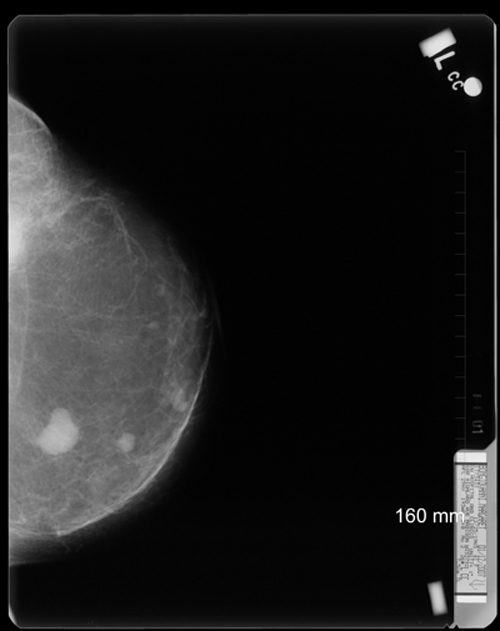
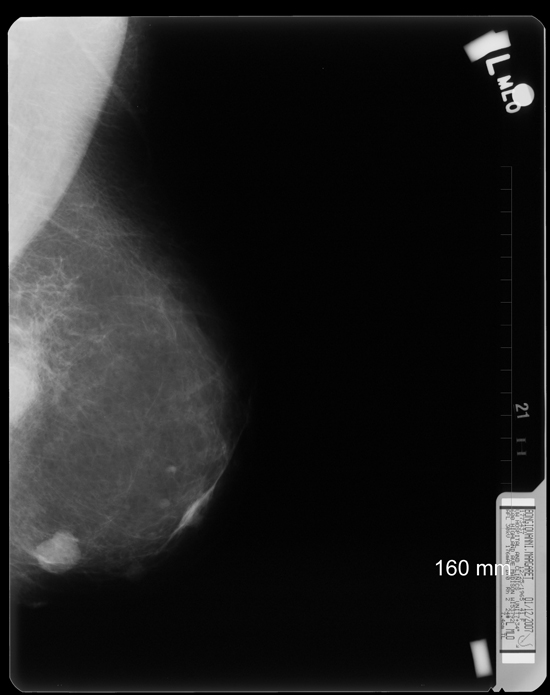
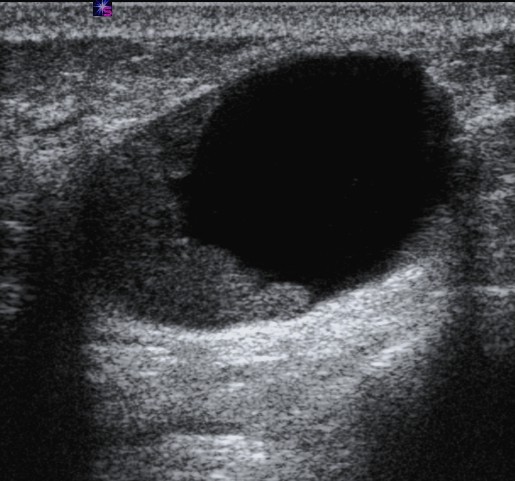
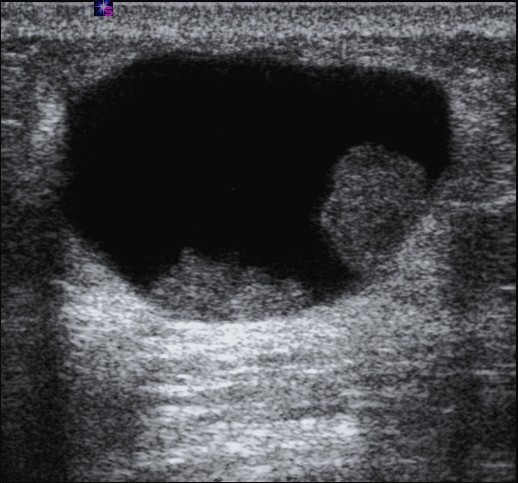
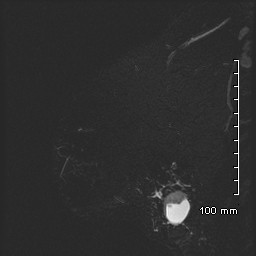
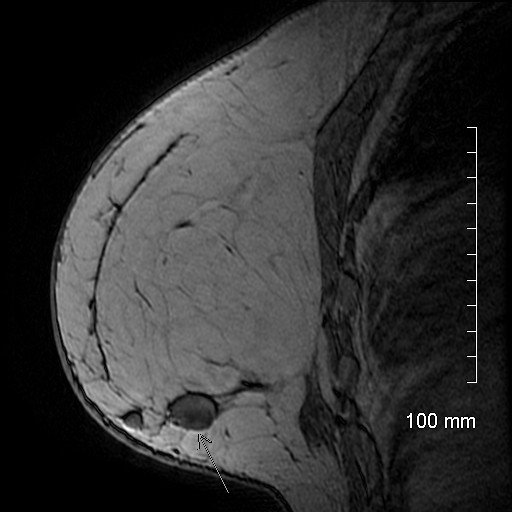
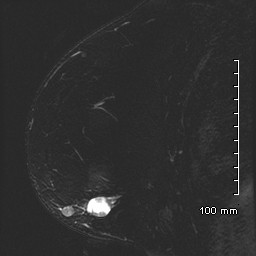
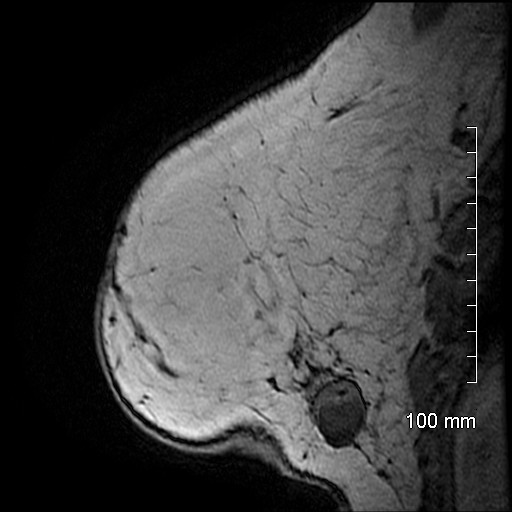
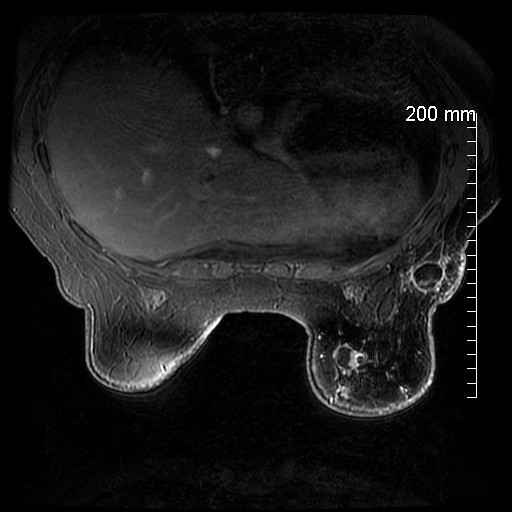
Approximately 50% of papillary carcinomas arise in the retroareolar portion of the breast. The most common mammographic appearance is a well-circumscribed round, oval or lobulated mass. Multiple masses may occur, often within one quadrant. Spiculation is an uncommon finding. Ultrasound typically demonstrates single or multiple masses with mixed cystic and solid components. Marked enhancement of cyst walls, septations and mural nodules is commonly seen on MRI. Lesions classified as papillary carcinoma are either intraductal or intracystic. Histology demonstrates frond-like arborization of fibrovascular stroma supporting the epithelial component. The absence of a myoepithelial layer differentiates carcinomas from benign papillary lesions.
In this case, a specific diagnosis is suggested based on the imaging findings. The differential diagnosis of a large circumscribed breast mass on mammography includes benign entities, including cyst, fibroadenoma, papilloma, hematoma, and abscess. Potentially malignant phyllodes tumors and malignant etiologies are also included, but occur rarely.
Ultrasound findings exclude solid masses like fibroadenomas and phyllodes tumors. The intracystic mural nodules on ultrasound and marked contrast enhancement on MRI are findings that take simple breast cyst, hematoma and abscess out of the differential. Multiple papillomas are unlikely given the location and lack of dilated ducts.
References: Liberman L, Feng TL, Susnik B: Case 35: Intracystic papillary carcinoma with invasion. Radiology 2001; 219:781-784.
Rosen PP: Papillary carcinoma, in Rosen’s Breast Pathology, 335-354. Philadelphia; Lippincott Williams & Wilkins; 1997.
Schneider JA. Invasive papillary breast carcinoma: mammographic and sonographic appearance. Radiology 1989; 171: 377-379.
Soo MS, Williford ME, Walsh R, Bentley RC, Kornguth PJ. Papillary carcinoma of the breast: imaging findings. AJR 1995; 164:321-326.
Many thanks to Jen Bergin for providing this case.
Approximately 50% of papillary carcinomas arise in the retroareolar portion of the breast. The most common mammographic appearance is a well-circumscribed round, oval or lobulated mass. Multiple masses may occur, often within one quadrant. Spiculation is an uncommon finding. Ultrasound typically demonstrates single or multiple masses with mixed cystic and solid components. Marked enhancement of cyst walls, septations and mural nodules is commonly seen on MRI. Lesions classified as papillary carcinoma are either intraductal or intracystic. Histology demonstrates frond-like arborization of fibrovascular stroma supporting the epithelial component. The absence of a myoepithelial layer differentiates carcinomas from benign papillary lesions.
In this case, a specific diagnosis is suggested based on the imaging findings. The differential diagnosis of a large circumscribed breast mass on mammography includes benign entities, including cyst, fibroadenoma, papilloma, hematoma, and abscess. Potentially malignant phyllodes tumors and malignant etiologies are also included, but occur rarely.
Ultrasound findings exclude solid masses like fibroadenomas and phyllodes tumors. The intracystic mural nodules on ultrasound and marked contrast enhancement on MRI are findings that take simple breast cyst, hematoma and abscess out of the differential. Multiple papillomas are unlikely given the location and lack of dilated ducts.
References: Liberman L, Feng TL, Susnik B: Case 35: Intracystic papillary carcinoma with invasion. Radiology 2001; 219:781-784.
Rosen PP: Papillary carcinoma, in Rosen’s Breast Pathology, 335-354. Philadelphia; Lippincott Williams & Wilkins; 1997.
Schneider JA. Invasive papillary breast carcinoma: mammographic and sonographic appearance. Radiology 1989; 171: 377-379.
Soo MS, Williford ME, Walsh R, Bentley RC, Kornguth PJ. Papillary carcinoma of the breast: imaging findings. AJR 1995; 164:321-326.
Many thanks to Jen Bergin for providing this case.