
Among the most ambitious medical imaging projects in history, the Human Connectome Project (HCP) aims to map the neural pathways that underlie human brain function. Using several imaging modalities and behavioral data, the project has already yielded valuable information about connectivity between brain networks.
While the main thrust of the project is the young adult connectome (ages 22-35), the National Institutes of Health (NIH) are launching additional grants to map connectomes affected by disease or injury, such as Alzheimer’s or traumatic brain injury. One such grant was recently awarded to a consortium consisting of UW-Madison and the Medical College of Wisconsin (MCW), to collect data for an epilepsy connectome. This is an NIH U01 Award of four years totaling greater than $5 Million.
Vivek Prabhakaran, M.D., Ph.D., is serving as a co-investigator on the project, while the overall primary investigator is MCW Professor of Neurology Jeff Binder, M.D. Additional investigators from UW include Professor of Medical Physics Elizabeth Meyerand, Ph.D., Professors of Neurology Rama Maganti, M.D. and Bruce Hermann, Ph.D., and Assistant Professor of Psychiatry Rasmus Birn, Ph.D.
This UW-MCW consortium grant is focused on temporal lobe epilepsy (TLE), a form of epilepsy where seizures originate from the temporal lobe of the brain. While MCW is the primary site for the grant, the workload is split evenly across both institutions.
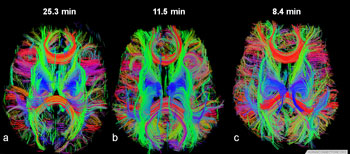
The data collection will follow a similar format to the HCP, but adjusted for the unique characteristics of epileptic brains, according to Dr. Prabhakaran. Functional Magnetic Resonance Imaging (fMRI) will produce information about functional connectivity, while Diffusion Tensor Imaging (DTI) will produce information about structural connectivity. In addition, brain activity will be mapped using Magnetoencephalography (MEG), a neuroimaging technique that records magnetic fields produced by electrical currents in the brain.
“MEG is even more important for our research, because MEG signatures play a large role in the diagnosis of epilepsy,” said Dr. Prabhakaran. Other changes from the standard HCP protocol include additional language and behavioral tasks specific to epilepsy.
“Memory and language are much more relevant in terms of epilepsy patients, but those weren’t the biggest focus for the overall HCP project,” said Dr. Prabhakaran.
While epilepsy researchers have increasingly explored how connections between brain regions may explain how seizures start in the first place, this study promises to set a new standard for collecting brain network data.
“I think it will be a paradigm shift. With the level and quality of data, this is the most detailed epilepsy brain connectome study ever conducted,” said Dr. Prabhakaran. “There’s going to be exquisite data that didn’t exist before, and it can provide us with a different understanding of the epilepsy syndrome.”
Dr. Prabhakaran hypothesizes that while TLE may arise in the temporal lobe, the entire brain is in fact abnormal. Misfires originating in the temporal lobe may affect the entire brain over time, causing the whole brain to be aberrant. Using millisecond resolution MEG and advanced MRI techniques, the researchers may be able to see that a large part of the brain is abnormal.
This may result in more subsets of TLE patients, based on levels of brain abnormality. More patients might have more diseased areas of the brain, while fewer patients might have diseased areas just localized to the temporal lobe, according to Dr. Prabhakaran.
These revelations could notably improve outcomes for TLE patients. Currently, most cases of TLE are lumped together as a single condition, so treatment options usually include specific surgeries or medication regimes.
“However, the diagnosis of additional sub-types of TLE may lead to different prognoses, and therefore different treatments,” said Dr. Prabhakaran. “If we are able to show that there are more subtypes of TLE, we can improve diagnosis and prognosis, and improve treatment options.”