More than 32.5 million adults in the United States suffer from osteoarthritis (OA), a joint disorder with causes pain, limited joint mobility, and psychological distress. In many cases, knee replacement surgery (also called “total knee arthroplasty” or TKA) is a highly effective treatment to reduce pain. But for some patients suffering from OA, knee replacement surgery isn’t an option.
Genicular nerve ablation (GNA) offers hope – and pain relief – to patients who aren’t surgical candidates.
“Some patients need to lose weight to be surgical candidates, which is hard to do when disabled by knee pain,” explains John Symanski, MD, the Director of the Advanced Osteoarthritis Ablation (AOA) clinical program. “Our most common type of patient is someone who needs to lose weight for knee arthroplasty and does not have pain relief with steroid injections.”
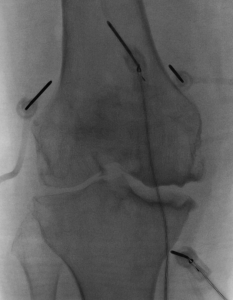
Unlike knee replacement surgery, GNA is minimally invasive. In this procedure, a probe delivers radiofrequency energy into the nerves surrounding the knee joint. These nerves are responsible for transmitting the pain signal. By disrupting this process, GNA alleviates the patient’s pain.
“There are currently three types of radiofrequency ablation instruments,” explains Dr. Symanski. “Here at UW, we use cooled radiofrequency ablation, a newer-generation technology, which is able to ablate a larger amount of tissue. This should theoretically lead to better outcomes, like more pain relief and longer-lasting pain relief.”
The Department of Radiology started offering GNA in February of 2023. Since then, Dr. Symanski has performed the procedure on 12 patients – for some of them, on both knees. While he’s performed all of the GNA’s so far, it has taken a team of people to get the program up and running: Kenneth Lee, MD, MBA, the Section Chief of Musculoskeletal Imaging and Intervention, Humberto Rosas, MD, the Director of Musculoskeletal Procedures, Erica Timm, RN, the clinical program coordinator, and the X-Ray technologists.
“Most patients have substantial pain relief for at least 6 months, with many patients still benefiting from pain relief at the one-year mark,” says Dr. Symanski.
While GNA has been around for many years, the procedural techniques and possibilities continue to evolve. With newer technology (such as cooled-RF), adding nerve targets, and refining the location of nerve targets, the procedure will continue to become more effective. Already, the field is expanding to other large joints such as the shoulder and hip, which can also be affected by OA.
“We are a developing program and only offer knee ablation at this time, but we may expand to other joints in the future,” says Dr. Symanski.