Saturday, April 25, 2026
8:00AM-12:00PM
Health Sciences Learning Center
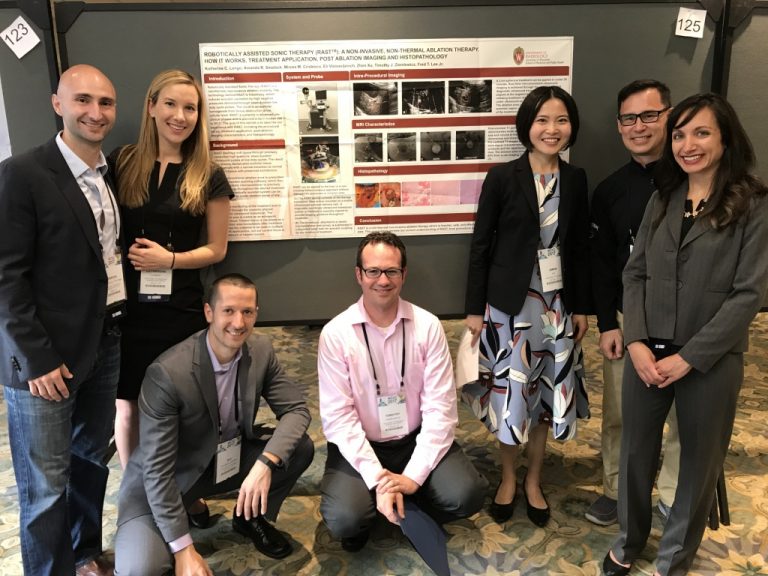
Sponsored by the UW Department of Radiology, the annual Zachary Clark Radiology Research Symposium held in spring celebrates the high-caliber radiology research conducted by our medical students, residents, and fellows. It also embodies the department’s dedication to both research and education.
Mark your calendars for April 25, 2026 when our residents, fellows and medical schools will present their newest research!
Symposium Details
Program & Keynote Speaker
Program Schedule
| 8:00 – 8:30AM | Continental Breakfast |
| 8:30 – 8:45AM | Welcome & Introduction Christoph Lee, MD, MS, MBA, Vice Chair or Research Allison Grayev, MD, Co-Moderator Venkata (Vinny) Meduri, MD, Co-Moderator |
| 8:45 – 10:15AM | Oral Presentations |
| 10:15 – 10:45AM | Electronic Exhibits Viewing |
| 10:45 – 11:45AM | Keynote Address Christopher Hess, MD, PhD |
| 11:45AM – Noon | Recognitions & Concluding Remarks |
Keynote Speaker
Christopher Hess, MD, PhD
Alexander R. Margulis Distinguished
Professor and Chair
Department of Radiology and Biomedical Imaging
UC San Francisco
Faculty MC's & Judges
Each year, faculty members volunteer to emcee the event as well as evaluate the oral presentations and electronic exhibits showcased at our symposium. We want to thank them for the time and thought they give to this endeavor.
Electronic Exhibit Judges
In Memoriam
This symposium honors the memory of Zachary Clark, MD, a former radiology resident known for his excellent clinician skills, kindness, and enthusiasm for research. Neuroradiology was his primary focus, especially cerebrovascular disease research.
In the spirit of his passion for research, we dedicate this symposium to Dr. Zachary Clark.
Support Resident Research
Attending the Zachary Clark Radiology Research Symposium is only one way to support research endeavors by residents and fellows. You can also make a gift to the Zachary Clark Resident Research Fund. Established in memory of Dr. Zachary Clark, January 25, 1986 – March 6, 2017, this endowment supports research performed by the UW School of Medicine and Public Health Radiology residents and ACGME-accredited fellows.

